From Wikipedia, the free encyclopedia
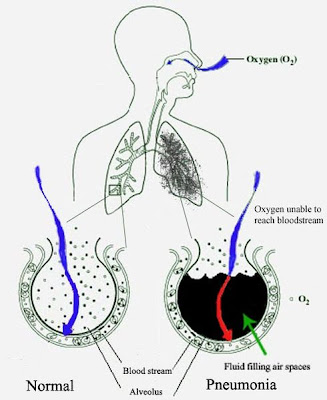
Pneumonia is an abnormal inflammatory condition of the lung.[1] It is often characterized as including inflammation of the parenchyma of the lung (that is, the alveoli) and abnormal alveolar filling with fluid (consolidation and exudation).[2]The alveoli are microscopic air-filled sacs in the lungs responsible for absorbing oxygen. Pneumonia can result from a variety of causes, including infection with bacteria, viruses, fungi, or parasites, and chemical or physical injury to the lungs. Its cause may also be officially described as idiopathic—that is, unknown—when infectious causes have been excluded.
Typical symptoms associated with pneumonia include cough, chest pain, fever, and difficulty in breathing. Diagnostic tools include x-rays and examination of the sputum. Treatment depends on the cause of pneumonia; bacterial pneumonia is treated with antibiotics.
Pneumonia is a common illness which occurs in all age groups, and is a leading cause of death among the elderly and people who are chronically and terminally ill. Additionally, it is the leading cause of death in children under five years old worldwide.[3] Vaccines to prevent certain types of pneumonia are available. The prognosis depends on the type of pneumonia, the appropriate treatment, any complications, and the person's underlying health.
Classification
Pneumonias can be classified in several ways. Pathologists originally classified them according to the anatomic changes that were found in the lungs during autopsies. As more became known about the microorganisms causing pneumonia, a microbiologic classification arose, and with the advent of x-rays, a radiological classification. Another important system of classification is the combined clinical classification, which combines factors such as age, risk factors for certain microorganisms, the presence of underlying lung disease and underlying systemic disease, and whether the person has recently been hospitalized.
Other types of pneumonia
- SARS is a highly contagious and deadly type of pneumonia which first occurred in 2002 after initial outbreaks in China. SARS is caused by the SARS coronavirus, a previously unknown pathogen.
- BOOP is caused by inflammation of the small airways of the lungs. It is also known as cryptogenic organizing pneumonitis (COP).
- Eosinophilic pneumonia is invasion of the lung by eosinophils, a particular kind of white blood cell. Eosinophilic pneumonia often occurs in response to infection with a parasite or after exposure to certain types of environmental factors.
- Chemical pneumonia (usually called chemical pneumonitis) is caused by chemical toxicants such as pesticides, which may enter the body by inhalation or by skin contact. When the toxic substance is an oil, the pneumonia may be called lipoid pneumonia.
- Aspiration pneumonia (or aspiration pneumonitis) is caused by aspirating foreign objects which are usually oral or gastric contents, either while eating, or after reflux or vomiting which results in bronchopneumonia. The resulting lung inflammation is not an infection but can contribute to one, since the material aspirated may contain anaerobic bacteria or other unusual causes of pneumonia. Aspiration is a leading cause of death among hospital and nursing home patients, since they often cannot adequately protect their airways and may have otherwise impaired defenses.
- Dust pneumonia describes disorders caused by excessive exposure to dust storms, particularly during the Dust Bowl in the United States. With dust pneumonia, dust settles all the way into the alveoli of the lungs, stopping the cilia from moving and preventing the lungs from ever clearing themselves.
- Necrotizing pneumonia, although overlapping with many other classifications, includes pneumonias that cause substantial necrosis of lung cells, and sometimes even lung abscess. Implicated bacteria are extremely commonly anaerobic bacteria, with or without additional facultatively anaerobic ones like Staphylococcus aureus, Klebsiella pneumoniae and Streptococcus pyogenes.[5] Type 3 pneumococcus is uncommonly implicated.[5]
- Opportunistic pneumonia includes those that frequently strike immunocompromised victims. Main pathogens are cytomegalovirus, Pneumocystis jiroveci, Mycobacterium avium-intracellulare, invasive aspergillosis, invasive candidiasis, as well as the "usual bacteria" that strike immunocompetent people as well.[5]
Signs and symptoms
People with infectious pneumonia often have a cough producing greenish or yellow sputum, or phlegm and a high fever that may be accompanied by shaking chills. Shortness of breath is also common, as is pleuritic chest pain, a sharp or stabbing pain, either experienced during deep breaths or coughs or worsened by them. People with pneumonia may cough up blood, experience headaches, or develop sweaty and clammy skin. Other possible symptoms are loss of appetite, fatigue, blueness of the skin, nausea, vomiting, mood swings, and joint pains or muscle aches. Less common forms of pneumonia can cause other symptoms; for instance, pneumonia caused by Legionella may cause abdominal pain and diarrhea, while pneumonia caused by tuberculosis or Pneumocystis may cause only weight loss and night sweats. In elderly people manifestations of pneumonia may not be typical. They may develop a new or worsening confusion or may experience unsteadiness, leading to falls. Infants with pneumonia may have many of the symptoms above, but in many cases they are simply sleepy or have a decreased appetite.
Symptoms of pneumonia need immediate medical evaluation. Physical examination by a health care provider may reveal fever or sometimes low body temperature, an increased respiratory rate, low blood pressure, a high heart rate, or a low oxygen saturation, which is the amount of oxygen in the blood as indicated by either pulse oximetry or blood gas analysis. People who are struggling to breathe, who are confused, or who have cyanosis (blue-tinged skin) require immediate attention.Physical examination of the lungs may be normal, but often shows decreased expansion of the chest on the affected side, bronchial breathing on auscultation with a stethoscope (harsher sounds from the larger airways transmitted through the inflamed and consolidated lung), and rales (or crackles) heard over the affected area during inspiration. Percussion may be dulled over the affected lung, but increased rather than decreased vocal resonance (which distinguishes it from a pleural effusion).[8] While these signs are relevant, they are insufficient to diagnose or rule out a pneumonia; moreover, in studies it has been shown that two doctors can arrive at different findings on the same patient.
Cause
Pneumonia can be caused by microorganisms, irritants and unknown causes. When pneumonias are grouped this way, infectious causes are the most common type.The symptoms of infectious pneumonia are caused by the invasion of the lungs by microorganisms and by the immune system's response to the infection. Although more than one hundred strains of microorganism can cause pneumonia, only a few are responsible for most cases. The most common causes of pneumonia are viruses and bacteria. Less common causes of infectious pneumonia are fungi and parasites.
Diagnosis
If pneumonia is suspected on the basis of a patient's symptoms and findings from physical examination, further investigations are needed to confirm the diagnosis. Information from a chest X-ray and blood tests are helpful, and sputum cultures in some cases. The chest X-ray is typically used for diagnosis in hospitals and some clinics with X-ray facilities. However, in a community setting (general practice), pneumonia is usually diagnosed based on symptoms and physical examination alone.[citation needed] Diagnosing pneumonia can be difficult in some people, especially those who have other illnesses. Occasionally a chest CT scan or other tests may be needed to distinguish pneumonia from other illnesses.
Investigations
An important test for pneumonia in unclear situations is a chest x-ray. Chest x-rays can reveal areas of opacity (seen as white) which represent consolidation. Pneumonia is not always seen on x-rays, either because the disease is only in its initial stages, or because it involves a part of the lung not easily seen by x-ray. In some cases, chest CT (computed tomography) can reveal pneumonia that is not seen on chest x-ray. X-rays can be misleading, because other problems, like lung scarring and congestive heart failure, can mimic pneumonia on x-ray.[12] Chest x-rays are also used to evaluate for complications of pneumonia (see below.)If antibiotics fail to improve the patient's health, or if the health care provider has concerns about the diagnosis, a culture of the person's sputum may be requested. Sputum cultures generally take at least two to three days, so they are mainly used to confirm that the infection is sensitive to an antibiotic that has already been started. A blood sample may similarly be cultured to look for bacteria in the blood. Any bacteria identified are then tested to see which antibiotics will be most effective.
A complete blood count may show a high white blood cell count, indicating the presence of an infection or inflammation. In some people with immune system problems, the white blood cell count may appear deceptively normal. Blood tests may be used to evaluate kidney function (important when prescribing certain antibiotics) or to look for low blood sodium. Low blood sodium in pneumonia is thought to be due to extra anti-diuretic hormone produced when the lungs are diseased (SIADH). Specific blood serology tests for other bacteria (Mycoplasma, Legionella and Chlamydophila) and a urine test for Legionella antigen are available. Respiratory secretions can also be tested for the presence of viruses such as influenza, respiratory syncytial virus, and adenovirus. Liver function tests should be carried out to test for damage caused by sepsis.
Prevention
There are several ways to prevent infectious pneumonia. Appropriately treating underlying illnesses (such as AIDS) can decrease a person's risk of pneumonia. Smoking cessation is important not only because it helps to limit lung damage, but also because cigarette smoke interferes with many of the body's natural defenses against pneumonia.Research shows that there are several ways to prevent pneumonia in newborn infants. Testing pregnant women for Group B Streptococcus and Chlamydia trachomatis, and then giving antibiotic treatment if needed, reduces pneumonia in infants. Suctioning the mouth and throat of infants with meconium-stained amniotic fluid decreases the rate of aspiration pneumonia.
Vaccination is important for preventing pneumonia in both children and adults. Vaccinations against Haemophilus influenzae and Streptococcus pneumoniae in the first year of life have greatly reduced the role these bacteria play in causing pneumonia in children. Vaccinating children against Streptococcus pneumoniae has also led to a decreased incidence of these infections in adults because many adults acquire infections from children. Hib vaccine is now widely used around the globe. The childhood pneumococcal vaccine is still as of 2009 predominantly used in high-income countries, though this is changing. In 2009, Rwanda became the first low-income country to introduce pneumococcal conjugate vaccine into their national immunization program.[16]
A vaccine against Streptococcus pneumoniae is also available for adults. In the U.S., it is currently recommended for all healthy individuals older than 65 and any adults with emphysema, congestive heart failure, diabetes mellitus, cirrhosis of the liver, alcoholism, cerebrospinal fluid leaks, or those who do not have a spleen. A repeat vaccination may also be required after five or ten years.[17]
Influenza vaccines should be given yearly to the same individuals who receive vaccination against Streptococcus pneumoniae. In addition, health care workers, nursing home residents, and pregnant women should receive the vaccine.[18] When an influenza outbreak is occurring, medications such as amantadine, rimantadine, zanamivir, and oseltamivir can help prevent influenza.
Treatment
Most cases of pneumonia can be treated without hospitalization. Typically, oral antibiotics, rest, fluids, and home care are sufficient for complete resolution. However, people with pneumonia who are having trouble breathing, people with other medical problems, and the elderly may need more advanced treatment. If the symptoms get worse, the pneumonia does not improve with home treatment, or complications occur, the person will often have to be hospitalized.Bacterial pneumonia
Antibiotics are used to treat bacterial pneumonia. In contrast, antibiotics are not useful for viral pneumonia, although they sometimes are used to treat or prevent bacterial infections that can occur in lungs damaged by a viral pneumonia.[citation needed] The antibiotic choice depends on the nature of the pneumonia, the most common microorganisms causing pneumonia in the local geographic area, and the immune status and underlying health of the individual. Treatment for pneumonia should ideally be based on the causative microorganism and its known antibiotic sensitivity. However, a specific cause for pneumonia is identified in only 50% of people, even after extensive evaluation.[citation needed] Because treatment should generally not be delayed in any person with a serious pneumonia, empiric treatment is usually started well before laboratory reports are available. In the United Kingdom, amoxicillin and clarithromycin or erythromycin are the antibiotics selected for most patients with community-acquired pneumonia; patients allergic to penicillins are given erythromycin instead of amoxicillin.[21] In North America, where the "atypical" forms of community-acquired pneumonia are becoming more common, macrolides (such as azithromycin and clarithromycin), the fluoroquinolones, and doxycycline have displaced amoxicillin as first-line outpatient treatment for community-acquired pneumonia.[22] The duration of treatment has traditionally been seven to ten days, but there is increasing evidence that shorter courses (as short as three days) are sufficient.[23][24][25]Antibiotics for hospital-acquired pneumonia include third- and fourth-generation cephalosporins, carbapenems, fluoroquinolones, aminoglycosides, and vancomycin.[26] These antibiotics are usually given intravenously. Multiple antibiotics may be administered in combination in an attempt to treat all of the possible causative microorganisms. Antibiotic choices vary from hospital to hospital because of regional differences in the most likely microorganisms, and because of differences in the microorganisms' abilities to resist various antibiotic treatments.
People who have difficulty breathing due to pneumonia may require extra oxygen. Extremely sick individuals may require intensive care, often including endotracheal intubation and artificial ventilation.
Over the counter cough medicine has not been found to be helpful in pneumonia.[27]






No comments:
Post a Comment