From Wikipedia, the free encyclopedia
Sepsis is a serious medical condition that is characterized by a whole-body inflammatory state (called a systemic inflammatory response syndrome or SIRS) and the presence of a known or suspected infection.[1][2] The body may develop this inflammatory response to microbes in the blood, urine, lungs, skin, or other tissues. An incorrect layman's term for sepsis is blood poisoning, more aptly applied to Septicemia, below.Septicemia (also septicaemia or septicæmia [sep⋅ti⋅cæ⋅mi⋅a][3], or erroneously Septasemia and Septisema) is a related but deprecated (formerly sanctioned) medical term referring to the presence of pathogenic organisms in the blood-stream, leading to sepsis.[4] The term has not been sharply defined. It has been inconsistently used in the past by medical professionals, for example as a synonym of bacteremia, causing some confusion. The present medical consensus is therefore that the term "septicemia" is problematic and should be avoided.[2]
Sepsis is usually treated in the intensive care unit with intravenous fluids and antibiotics. If fluid replacement is insufficient to maintain blood pressure, specific vasopressor drugs can be used. Artificial ventilation and dialysis may be needed to support the function of the lungs and kidneys, respectively. To guide therapy, a central venous catheter and an arterial catheter may be placed. Sepsis patients require preventive measures for deep vein thrombosis, stress ulcers and pressure ulcers, unless other conditions prevent this. Some patients might benefit from tight control of blood sugar levels with insulin (targeting stress hyperglycemia), low-dose corticosteroids or activated drotrecogin alfa
Signs and symptoms
In addition to symptoms related to the provoking infection, sepsis is characterized by evidence of acute inflammation present throughout the entire body, and is, therefore, frequently associated with fever and elevated white blood cell count (leukocytosis) or low white blood cell count and lower-than-average temperature, and vomiting[citation needed]. The modern concept of sepsis is that the host's immune response to the infection causes most of the symptoms of sepsis, resulting in hemodynamic consequences and damage to organs. This host response has been termed systemic inflammatory response syndrome (SIRS) and is characterized by hemodynamic compromise and resultant metabolic derangement. Outward physical symptoms of this response frequently include a high heart rate (above 100 beats per minute), high respiratory rate (above 20 breaths per minute), elevated WBC count (above 12,000) and elevated or lowered body temperature (under 36 °C or over 38 °C). Sepsis is differentiated from SIRS by the presence of a known pathogen. For example SIRS and a positive blood culture for a pathogen indicates the presence of sepsis. Without a known infection you can not classify the above symptoms as sepsis, only SIRS.This immunological response causes widespread activation of acute-phase proteins, affecting the complement system and the coagulation pathways, which then cause damage to the vasculature as well as to the organs. Various neuroendocrine counter-regulatory systems are then activated as well, often compounding the problem. Even with immediate and aggressive treatment, this may progress to multiple organ dysfunction syndrome and eventually death.
Definition
According to the American College of Chest Physicians and the Society of Critical Care Medicine[2], there are different levels of sepsis:- Systemic inflammatory response syndrome (SIRS). Defined by the presence of two or more of the following findings:
- Body temperature < 36 °C (97 °F) or > 38 °C (100 °F) (hypothermia or fever).
- Heart rate > 100 beats per minute (tachycardia).
- Respiratory rate > 20 breaths per minute or, on blood gas, a PaCO2 less than 32 mm Hg (4.3 kPa) (tachypnea or hypocapnia due to hyperventilation).
- White blood cell count < 4,000 cells/mm3 or > 12,000 cells/mm3 (< 4 × 109 or > 12 × 109 cells/L), or greater than 10% band forms (immature white blood cells). (leukopenia, leukocytosis, or bandemia).
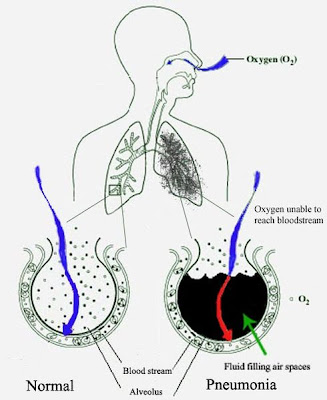
- Sepsis. Defined as SIRS in response to a confirmed infectious process. Infection can be suspected or proven (by culture, stain, or polymerase chain reaction (PCR)), or a clinical syndrome pathognomonic for infection. Specific evidence for infection includes WBCs in normally sterile fluid (such as urine or cerebrospinal fluid (CSF), evidence of a perforated viscus (free air on abdominal x-ray or CT scan, signs of acute peritonitis), abnormal chest x-ray (CXR) consistent with pneumonia (with focal opacification), or petechiae, purpura, or purpura fulminans
- Severe sepsis. Defined as sepsis with organ dysfunction, hypoperfusion, or hypotension.
- Septic shock. Defined as sepsis with refractory arterial hypotension or hypoperfusion abnormalities in spite of adequate fluid resuscitation. Signs of systemic hypoperfusion may be either end-organ dysfunction or serum lactate greater than 4 mmol/dL. Other signs include oliguria and altered mental status. Patients are defined as having septic shock if they have sepsis plus hypotension after aggressive fluid resuscitation (typically upwards of 6 liters or 40 ml/kg of crystalloid).
- Lungs
- acute lung injury (ALI) (PaO2/FiO2 < 300) or acute respiratory distress syndrome (ARDS) (PaO2/FiO2 < 200)
- Brain
- encephalopathy
- symptoms:
- agitation
- confusion
- coma
- etiologies:
- ischemia
- hemorrhage
- microthrombi
- microabscesses
- multifocal necrotizing leukoencephalopathy
- symptoms:
- encephalopathy
- Liver
- disruption of protein synthetic function: manifests acutely as progressive coagulopathy due to inability to synthesize clotting factors
- disruption of metabolic functions: manifests as cessation of bilirubin metabolism, resulting in elevated unconjugated serum bilirubin levels (indirect bilirubin)
- Kidney
- Heart
- systolic and diastolic heart failure, likely due to cytokines that depress myocyte function
- cellular damage, manifest as a troponin leak (although not necessarily ischemic in nature)
- Cardiovascular dysfunction (after fluid resuscitation with at least 40 ml/kg of crystalloid)
- hypotension with blood pressure < 5th percentile for age or systolic blood pressure < 2 standard deviations below normal for age, OR
- vasopressor requirement, OR
- two of the following criteria:
- unexplained metabolic acidosis with base deficit > 5 mEq/L
- lactic acidosis: serum lactate 2 times the upper limit of normal
- oliguria (urine output < 0.5 ml/kg/hr)
- prolonged capillary refill > 5 seconds
- core to peripheral temperature difference > 3°C
- Respiratory dysfunction (in the absence of cyanotic heart disease or known chronic lung disease)
- the ratio of the arterial partial-pressure of oxygen to the fraction of oxygen in the gases inspired (PaO2/FiO2) < 300 (the definition of acute lung injury), OR
- arterial partial-pressure of carbon dioxide (PaCO2) > 65 torr (20 mmHg) over baseline PaCO2 (evidence of hypercapnic respiratory failure), OR
- supplemental oxygen requirement of greater than FiO2 0.5 to maintain oxygen saturation ≥ 92%
- Neurologic dysfunction
- Glasgow Coma Score (GCS) ≤ 11, OR
- altered mental status with drop in GCS of 3 or more points in a patient with developmental delay/mental retardation
- Hematologic dysfunction
- platelet count < 80,000/mm3 or 50% drop from maximum in chronically thrombocytopenic patients, OR
- international normalized ratio (INR) > 2
- Disseminated Intravascular Coagulation
- Renal dysfunction
- serum creatinine ≥ 2 times the upper limit of normal for age or 2-fold increase in baseline creatinine in patients with chronic kidney disease
- Hepatic dysfunction (only applicable to infants > 1 month)
- total serum bilirubin ≥ 4 mg/dl, OR
- alanine aminotransferase (ALT) ≥ 2 times the upper limit of normal
Treatment
Adults and children
The therapy of sepsis rests on antibiotics, surgical drainage of infected fluid collections, fluid replacement and appropriate support for organ dysfunction. This may include hemodialysis in kidney failure, mechanical ventilation in pulmonary dysfunction, transfusion of blood products, and drug and fluid therapy for circulatory failure. Ensuring adequate nutrition—preferably by enteral feeding, but if necessary by parenteral nutrition—is important during prolonged illness.A problem in the adequate management of septic patients has been the delay in administering therapy after sepsis has been recognized. Published studies have demonstrated that for every hour delay in the administration of appropriate antibiotic therapy there is an associated 7% rise in mortality. A large international collaboration was established to educate people about sepsis and to improve patient outcomes with sepsis, entitled the "Surviving Sepsis Campaign." The Campaign has published an evidence-based review of management strategies for severe sepsis,[5] with the aim to publish a complete set of guidelines in subsequent years.
Early Goal Directed Therapy (EGDT), developed at Henry Ford Hospital by E. Rivers, MD, is a systematic approach to resuscitation that has been validated in the treatment of severe sepsis and septic shock. It is meant to be started in the Emergency Department. The theory is that one should use a step-wise approach, having the patient meet physiologic goals, to optimize cardiac preload, afterload, and contractility, thus optimizing oxygen delivery to the tissues.[13] A recent meta-analysis showed that EGDT provides a benefit on mortality in patients with sepsis.[14] As of December 2008 some controversy around its uses remains and a number of trials are ongoing in an attempt to resolve this.[15]
In EGDT, fluids are administered until the central venous pressure (CVP), as measured by a central venous catheter, reaches 8-12 cm of water (or 10-15 cm of water in mechanically ventilated patients). Rapid administration of several liters of isotonic crystalloid solution is usually required to achieve this. If the mean arterial pressure is less than 65 mmHg or greater than 90 mmHg, vasopressors or vasodilators are given as needed to reach the goal. Once these goals are met, the mixed venous oxygen saturation (SvO2), i.e., the oxygen saturation of venous blood as it returns to the heart as measured at the vena cava, is optimized. If the SvO2 is less than 70%, blood is given to reach a hemoglobin of 10 g/dl and then inotropes are added until the SvO2 is optimized. Elective intubation may be performed to reduce oxygen demand if the SvO2 remains low despite optimization of hemodynamics. Urine output is also monitored, with a minimum goal of 0.5 ml/kg/h. In the original trial, mortality was cut from 46.5% in the control group to 30.5% in the intervention group.[13] The Surviving Sepsis Campaign guidelines recommend EGDT for the initial resuscitation of the septic patient with a level B strength of evidence (single randomized control trial).[5]
Most therapies aimed at the inflammation process itself have failed to improve outcome, however drotrecogin alfa (activated protein C, one of the coagulation factors) has been shown to decrease mortality from about 31% to about 25% in severe sepsis. To qualify for drotrecogin alfa, a patient must have severe sepsis or septic shock with an APACHE II score of 25 or greater and a low risk of bleeding.[16]
During critical illness, a state of adrenal insufficiency and tissue resistance (the word 'relative' resistance should be avoided[17]) to corticosteroids may occur. This has been termed critical illness–related corticosteroid insufficiency.[17] Treatment with corticosteroids might be most beneficial in those with septic shock and early severe acute respiratory distress syndrome (ARDS), whereas its role in other patients such as those with pancreatitis or severe pneumonia is unclear.[17] These recommendations stem from studies showing benefits from low dose hydrocortisone treatment for septic shock patients and methylprednisolone in ARDS patients.[18][19][20][21][22][23] However, the exact way of determining corticosteroid insufficiency remains problematic. It should be suspected in those poorly responding to resuscitation with fluids and vasopressors. ACTH stimulation testing is not recommended to confirm the diagnosis.[17] Glucocorticoid drugs should be weaned and not stopped abruptly.
In some cases, sepsis may lead to inadequate tissue perfusion and necrosis. As this may affect the extremities, amputation may become necessary. On January 8 2009 a patent request was submitted for the possible treatment of sepsis ( 20090011974 Scavenger Receptor B1 (Cla-1) Targeting for the Treatment of Infection, Sepsis and Inflammation 01-08-2009) .